CIHIE helps local providers bridge communication gaps in one of the most significant transformations to happen in healthcare.
Ask any business that has undertaken a major software implementation about their experience, and you are likely to hear about significant anxieties that arose along the way:
- Did we choose the right software?
- Are we training people too early or too late?
- Is the system intuitive enough for staff to understand?
- What will the impact be on the customer experience?
- If productivity drops, even temporarily, how much will that cost us?
Healthcare organizations across central Illinois are facing exactly these questions as they embark on perhaps the most extensive modernization effort ever undertaken in medical records. Paper files that previously lined the walls of most offices are disappearing, replaced by software that staff accesses via desktop computers, tablets or mobile devices.
Such transitions are rarely easy, but the situation in healthcare is further complicated by shifting industry expectations. Hospitals and physician offices are purchasing and implementing software, while aiming for a moving target. In fact, what was satisfactory or even forward-thinking just a few short years ago is no longer sufficient.
Key funders such as Medicaid, Medicare and private insurers are insisting that patient records not only be electronic, but also seamlessly accessible across a variety of settings. However, the concept of seamless communication is not well suited to an industry in which local competition is fierce, smaller practices are being purchased and merged into larger institutions, and technology vendors are exclusionary and proprietary.
Collaboration Is the Only Choice
Proponents for technology improvements point to skyrocketing healthcare costs, driven in part by ineffective coordination. Quite simply, it is often easier for a physician to run new tests than it is to track down results from other providers. In addition, running tests and performing procedures have historically been billable activities which generate revenue. Relying on a test or procedure that was performed elsewhere does not.
With the advent of various payment models that employ both carrots (financial incentives) and sticks (financial penalties), healthcare providers are being forced into a brave new world—one which rewards making better coordinated care decisions.
Interestingly, the requirements being forced upon this highly competitive industry make it virtually impossible for any organization to achieve their goals alone. You simply cannot be a better-coordinated, better-informed healthcare provider without the help of your competitors. You only get better when they also get better. With time, we can expect that some organizations will become more sophisticated with interpreting and responding to available records, but for the immediate moment, organizations are relying on each other to move forward and meet minimum requirements.
Creating a Neutral Table
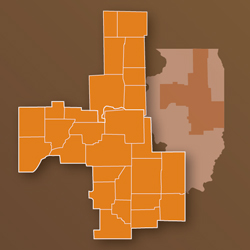
For communities like Peoria, Bloomington/Normal, Decatur, Champaign and Rockford, the key to making this transformation possible has been the creation of a neutral table around which competing healthcare organizations can gather and plan. After a year of initial discussions involving more than 200 people from organizations across a 20-county area, 11 charter members invested seed capital to launch Central Illinois Health Information Exchange, abbreviated as CIHIE and pronounced “See-High.”
As of this article’s publication, CIHIE has been operational for 18 months, serving as the conduit through which patient records can be securely transmitted among participating healthcare organizations. More than 2.9 million patient records are available for request through the exchange, with less than 0.02 percent of patients choosing to have their records excluded.
Participation has grown from the 11 initial members to more than 35 organizations, including most of the area’s hospitals, a number of specialty practices and nonprofit clinics, 30 long-term care facilities and a regional emergency medical services transportation provider. The outlook for additional growth in 2014 looks promising.
Real-World Results
While it’s still too early to measure collective regional results, clinicians can already cite examples in which a patient query has proven useful—and potentially even life-saving. One physician was faced with a patient who arrived at the emergency room in a confused mental state, unable to communicate what was happening. A search of the HIE revealed medical history that immediately provided the answer.
Another physician documented his findings during his normal process of seeing 40 consecutive patients. Of those 40 patients:
- Three had allergies or drug reactions that were not documented in their medical records. For one of those patients, he was able to intervene before the patient received the first dose of a medication that had been diagnosed as the cause of a significant neurological reaction elsewhere.
- Two patients had recently been subjected to duplicate tests.
- One patient had a recent echocardiogram that would have been duplicated to meet his hospital’s required congestive heart failure quality metrics had he not discovered that it had already been done at a different hospital.
- Four patients were unable to tell him their insulin dosages. He was able to find the dosages in the HIE, which helped him start them with a more accurate dose.
- One patient had a bowel procedure but couldn’t tell him what it was. He was able to discover the exact procedure through the HIE search.
- Five patients had significant problems, such as diabetic retinopathy, and one had even experienced a stroke. None of that information was available except through the HIE.
- Eight patients were missing immunizations that could not be found elsewhere. Knowing that information helped his own organization’s quality figures for flu shots and pneumovax.
- One patient told him he was seeing an endocrinologist for treatment of his diabetes, but the HIE revealed the patient’s last visit was actually more than three years earlier.
Updated information is accessible via the HIE in real time. In one Decatur example, an emergency room physician queried for a patient’s records and discovered that the patient had just left the emergency room of a hospital across town 15 minutes earlier.
What’s Next for the Region?
CIHIE’s founding members aim to maintain the HIE as a secure and neutral platform for collaboration. Work is underway to establish connectivity with similar exchanges in other parts of the state and nationally.
While businesses and other healthcare payers can look forward to seeing a financial benefit from better coordinated care, patients should experience improved portability of their healthcare records. The days of faxing and mailing files between medical offices will soon be behind us, as those records will be available securely with just a few clicks of the mouse.
This is undoubtedly one of the most significant transformations to happen in healthcare. You won’t see it happen overnight, but you will certainly notice change happening. iBi

